Structural Heart Clinic

Now through technology and medical expertise, these patients – such as an 86-year-old who experienced a catheter-based heart valve procedure – enjoy immediately getting back to a more active life.
“I had Cardiac Rehab call me and ask why the patient was not going to rehab,” recalls Linda Minor, BSN, RN, a nurse in the clinic. “I told them she felt so good she was going to yoga classes twice a week.”
The six-member Structural Heart Clinic team and their Medical Director Nicklaus Slocum, MD, FACC, FSCAI, work with cardiothoracic surgeons and other departments throughout the hospital to give patients with structural heart disease the opportunity to walk to the mailbox and get the mail again, play with grandchildren, and live a quality of life that keeps them out of the hospital.
“We try to look at the patient and their individual needs,” says Deb Provost, BSN, RN, clinic coordinator. “They are elderly and frail and we don’t just want them to live longer, but better.”
The clinic offers patients with severe heart valve abnormalities the opportunity to be seen by cardiologists, cardiothoracic surgeons, and nurses at the Webber Heart Center’s Cardio Diagnostic Suite. The team works to provide comprehensive patient treatment options for aortic stenosis, atrial fibrillation, mitral valve disease, perivalvular leaks, and other heart defects.
Advanced Procedures and Services
Advanced procedures and services available through the clinic include:
- Catheter replacement of an aortic valve (TAVR)
- Catheter-based repair of a mitral valve using the MitraClip® device
- Catheter-based left atrial appendage (LAA) closure for stroke prevention in atrial fibrillation patients using the WATCHMAN™ device
- Catheter-based closure of PFO and ASD (heart defects)
- Sentinel Cerebral Protection System
MitraClip®
Patients with leaking heart mitral valves who are not eligible for a surgical option to repair a valve now have hope through the MitraClip® device. A team that includes interventional cardiologists, cardiothoracic surgeons, cardiologists who specialize in echocardiography, anesthesiologists, and others will meet with patients in Munson Medical Center’s Structural Heart Clinic.
Patients cleared for the procedure have it performed in the hospital’s Cardiac Catheterization Lab. Patients are put under general anesthesia and the interventional cardiologist guides the catheter from a groin blood vessel up into the heart and across into the area of the mitral valve. Once the echocardiography experts and interventional cardiologists have the catheter into the right place in the heart, the team puts the tiny clip in place. Sometimes more than one clip is needed to stop the leaking. Patients stay 24 - 48 hours in the hospital for monitoring and return to see their cardiologist 30 days after the procedure.
“The feedback we hear from patients is that the procedure is simpler than they expected,” says Nicklaus Slocum, MD, FACC, FSCAI, an interventional cardiologist and medical director for the Structural Heart Clinic. “They also have been impressed with how fast they get back to feeling more like themselves.”
Watchman™ Device
The Watchman™ device represents heart care technology at Munson Medical Center that is helping reduce the risk of strokes for certain heart patients with atrial fibrillation or irregular heartbeats.
During the procedure, the small device is delivered through the vein in a leg to an appendage in the left atrium of the heart while the patient is under general anesthesia. The device seals off the appendage, preventing any blood clots from forming.
Research shows that one third of all strokes are due to atrial fibrillation. Medical evidence shows a marked decrease in disabling strokes for patients when the Watchman™ device is deployed. Munson Medical Center’s team began using the device in early 2018.
PFO and ASD Defects
Patent Formen Ovale (PFO) is a birth defect in the heart that allows blood to leak from the right atria into the left atria. Typically, these two upper chambers of the heart are closed off from one another after birth due to higher pressure in the left atria and lower in the right atria. Atrial septal defect (ASD) is the name for a hole in the septum that separates the upper chambers of the heart that allows blood to leak between the upper chambers.
Minimally invasive treatment for these conditions involves a catheter-based procedure that allows the cardiologist to place a device that acts as a plug into the hole to stop the leak between the upper chambers.
Sentinel® Cerebral Protection
Munson Medical Center was among the first hospitals in the country to introduce the Sentinel® Cerebral Protection System. The technology helps protect patients from the risk of stroke during minimally-invasive heart valve surgery, known as transcatheter aortic valve replacement (TAVR).
Use of cerebral protection devices takes an already safe and effective procedure and makes it even safer. The Sentinel system is the first FDA-cleared device available in the U.S. to capture and remove any dislodged calcium before it reaches the brain. The device has been shown to reduce strokes by 63 percent during the procedure and in the first 72 hours after it, when most strokes occur.
“Offering this technology is an example of the structural heart program and our cardiovascular services keeping the patient, their safety, and outcome, at the center of what we do,” said Nicklaus Slocum, MD, FACC, FSCAI, medical director for the Structural Heart Clinic.
Salvatore’s Story
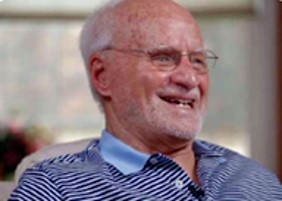
Salvatore could wait three months and have the procedure done at Munson, or he could go to another hospital and have it done immediately. Even though he was feeling weak and ill, Sal chose to wait.
On Sept. 12, Sal was the first patient to undergo a TAVR procedure at Munson Medical Center. “I had open heart surgery there 14 years ago. I wanted to stay with Munson – I like Munson, they are nice people, really nice people. Everyone is so concerned and kind.”
Sal, a native of Naples, Italy, had no qualms about being Munson’s first TAVR patient. “I was not really scared. I feel comfortable at Munson – I never say I go someplace else,” he said.
Sal is a retired barber who immigrated to the United States in 1956 to find a better life. He worked as a cement laborer before opening his own barbershop in Dearborn. He and his wife, Assunta, retired to northern Michigan in 1994 to be near their daughter and five grandchildren.
Sal first noticed his health diminishing while he and Assunta were wintering in Florida. “I usually walk five or six miles in the morning. In March 2012 I slowed down and by May it was worse. For the three months I was waiting for the TAVR, I couldn’t do much outside. Deb Provost (the Patient Care Coordinator at Munson’s Structural Heart Clinic) called me every week to tell me what’s going on – how close they were to being ready.”
Following the TAVR procedure, Sal said he feels like a new man. “I feel really perfect – like I was years ago. It’s like a miracle.”
Sal is eager to spend his winter mornings in Florida walking again. “Now I go in Florida and have a chance to be outdoors. I never was a couch potato – I like to move. I’m never going to get old.”